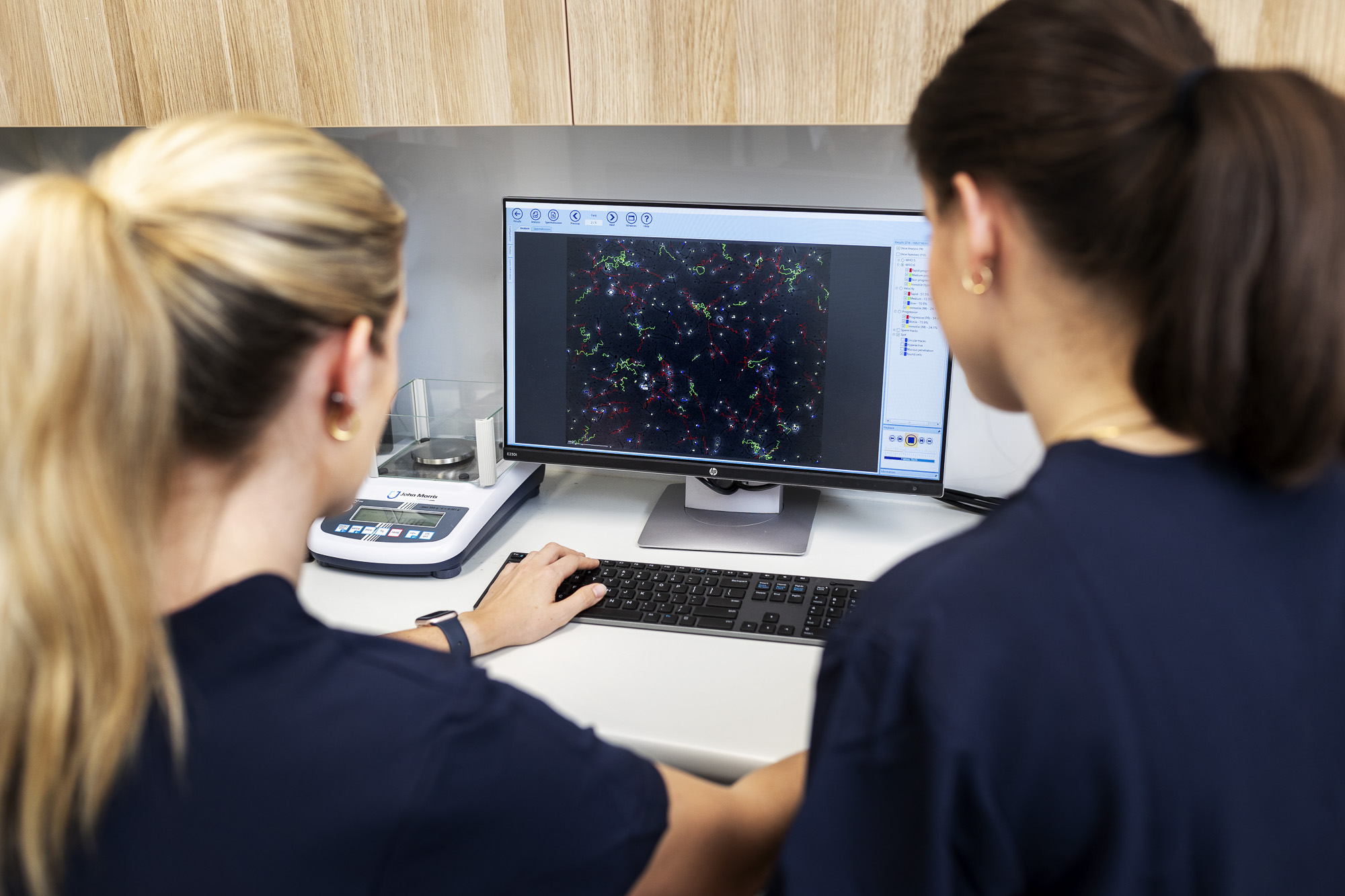
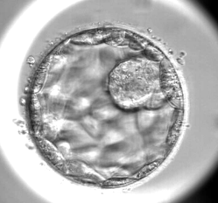
The lab environment aims to mimic the conditions your embryos would experience if they were growing in your reproductive tract. This includes the right oxygen pressure, temperature and nutrients, as required for all the different stages of development. In addition, we continuously monitor the growth of your embryos using time-lapse imaging. However, despite these efforts, some embryos may not progress to the blastocyst stage.
In this video, fertility specialist Dr Nicole Hope details some of the changes that take place when a fertilised egg develops into a blastocyst embryo.
Embryo arrest
Approximately 60% of fertilised eggs become blastocysts. This means that around 40% of embryos stop growing before becoming a day 5–6 embryo. This is known as embryo arrest and occurs when an embryo stops dividing for 24 hours.
Not all embryos that reach the blastocyst stage are suitable for embryo transfer or freezing, as they may not have all the components necessary to result in a healthy pregnancy. Generally, around 40–50% of fertilised eggs become blastocysts that we can transfer or freeze. However, this varies greatly depending on your age and medical history. There is also a small group of individuals who have poor embryo development, which may be due to developmental-specific events or a pattern of embryo progression. Most IVF patients experience embryo arrest in some form, and it is usually a protective mechanism for stopping the development of abnormal or poor-quality embryos.
Causes of embryo arrest
There are many reasons why an embryo might stop developing. The embryo could have reduced metabolic activity or slow development and as a result, degenerate. In addition, embryos can stop growing during different stages of development. They may fail to reach the blastocyst stage for several reasons discussed below.
Chromosomal errors
Around 70% of arrested embryos display chromosomal errors.1 Chromosomes are rope-like structures inside your cells that contain DNA – i.e. the instruction manual that makes you unique. When sperm and egg come together, the mother and father pass on 23 chromosomes each, so that the resulting embryo has a total of 46 chromosomes.
Sometimes, chromosomes can fail to combine correctly leading to chromosomal errors. This may include having:
- an abnormal number of chromosomes (called aneuploidy)
- more than one full set of chromosomes (called polyploidy)
- a combination of both normal and abnormal numbers of chromosomes (called mosaicism).
In addition, chromosomal errors can develop during the replication and division of the cells in the embryo. If an embryo divides abnormally during the early stages of its development (also known as the cleavage stage), this can lead to an abnormal distribution of chromosomes between cells and result in embryo arrest. Cells within the embryo can also have abnormal DNA replication and/or damaged DNA leading to embryo arrest.
Some chromosomal errors do not stop the embryo from growing, which is why preimplantation genetic screening (PGT) may be recommended.
Cell division errors
Usually, a cell within an embryo divides from one cell into two and distributes its chromosomes evenly. However, in some instances, a cell within an embryo divides from one cell to three. This is called Direct Uneven Cleavage (DUC). When DUC occurs in the first cell division, there is a higher chance of embryo arrest occurring.
The chances of embryo arrest occurring also depend on how much the cells are affected. Sometimes, an embryo may divide very quickly from one cell to two and three cells, and this rapid division can be difficult to differentiate from DUC. Under these circumstances, the rapidly dividing embryo has a greater chance of becoming a blastocyst.
Another cell division error can occur if the cell fails to divide but the nucleus (the information centre of all cells which contains your chromosomes and DNA) continues to replicate. This can lead to there being more than one complete set of chromosomes inside a single cell. If this occurs in several cells, the embryo will arrest; however, if this phenomenon is present only in a few cells, the embryo still has the potential to reach the blastocyst stage.
Poor embryo development
Early cleavage within the embryo relies on special products inside the egg to drive development. Sometimes, defects in the development of an embryo reflect the quality of the egg and can cause the embryo to stop dividing.
Embryos can also undergo instructed cell death (known as apoptosis). Apoptosis is a biological mechanism that aims to remove any unwanted or damaged cells from the embryo in its early stages of development. If enough apoptosis occurs, the embryo can fail to develop further.
Mitochondrial function
Mitochondria are like little organs inside a cell that act as a power supply. Specifically, they produce an energy-carrying molecule called ATP (short for adenosine triphosphate). Inherited only from the mother’s egg, mitochondria produce the energy that eggs and embryos need to function properly. During the early growth stages of an embryo, mitochondria undergo structural and positional changes that allow them to provide energy to the embryo and regulate their environment. These events are a key part of the development of an embryo before implantation takes place inside the womb.
As a woman ages, the quality of her eggs declines. Increasing maternal age can result in mitochondrial dysfunction due to changes or damage to the mitochondrial DNA – yes, mitochondria have DNA just like the nucleus of a cell. If the mitochondrial DNA is damaged, this can result in inadequate amounts of ATP or energy, as well as the loss of other important mitochondrial functions required following fertilisation. In addition, low mitochondrial DNA content is also associated with fertilisation failure and abnormal embryo development. Basically, if an egg or embryo does not have enough of a power supply, developmental processes will stop.
Between days two and three of embryo development, i.e. from the four-cell to the eight-cell stage, an embryo’s genome is activated. A genome refers to the genetic material (chromosomes containing DNA) inside a cell. When an embryo’s genome is activated, the embryo no longer relies on the egg to continue growing; rather, it uses its own cellular machinery. This change in embryonic genome activity is regulated by special products that mitochondria produce. Around 10% of embryos do not make the switch from maternal egg control to embryonic genome control. This means that an embryo on day two may be at the four-cell stage but fail to progress further if the genome switch does not occur.
Looking for more information?
There are many reasons why an embryo may not progress beyond a certain developmental stage. Throughout your cycle, our embryologists will phone you to keep you updated on the progress of your embryos. We know this can be an anxious time as you wait to hear how many of your eggs have been fertilised and then how many of these have developed into quality embryos suitable for transfer or freezing. If you have any concerns throughout this time, we encourage you to call us on (03) 8080 8933 for the extra support and information you need.
References
- Maurer M, Ebner T, Puchner M, et al. Chromosomal Aneuploidies and Early Embryonic Developmental Arrest. Int J Fertil Steril. 2015; 9(3):346-353. ↩