- My Journey
- Events
- Donors
- Appointments
-
- Legal disclaimer
- Privacy policy
- ©2024 Newlife IVF. All rights reserved. | Site designed by Wellmark
- About us
Book an appointment
If you’re interested in receiving fertility treatment at Newlife IVF or booking an appointment with one of our fertility specialists
T: (03) 8080 8933 - Team
Book an appointment
If you’re interested in receiving fertility treatment at Newlife IVF or booking an appointment with one of our fertility specialists
T: (03) 8080 8933 - Services
- Fertility testing
- Early fertility treatment
- IVF services
- Preimplantation genetic testing (PGT)
- Fertility preservation
- Donor and surrogacy
Book an appointment
If you’re interested in receiving fertility treatment at Newlife IVF or booking an appointment with one of our fertility specialists
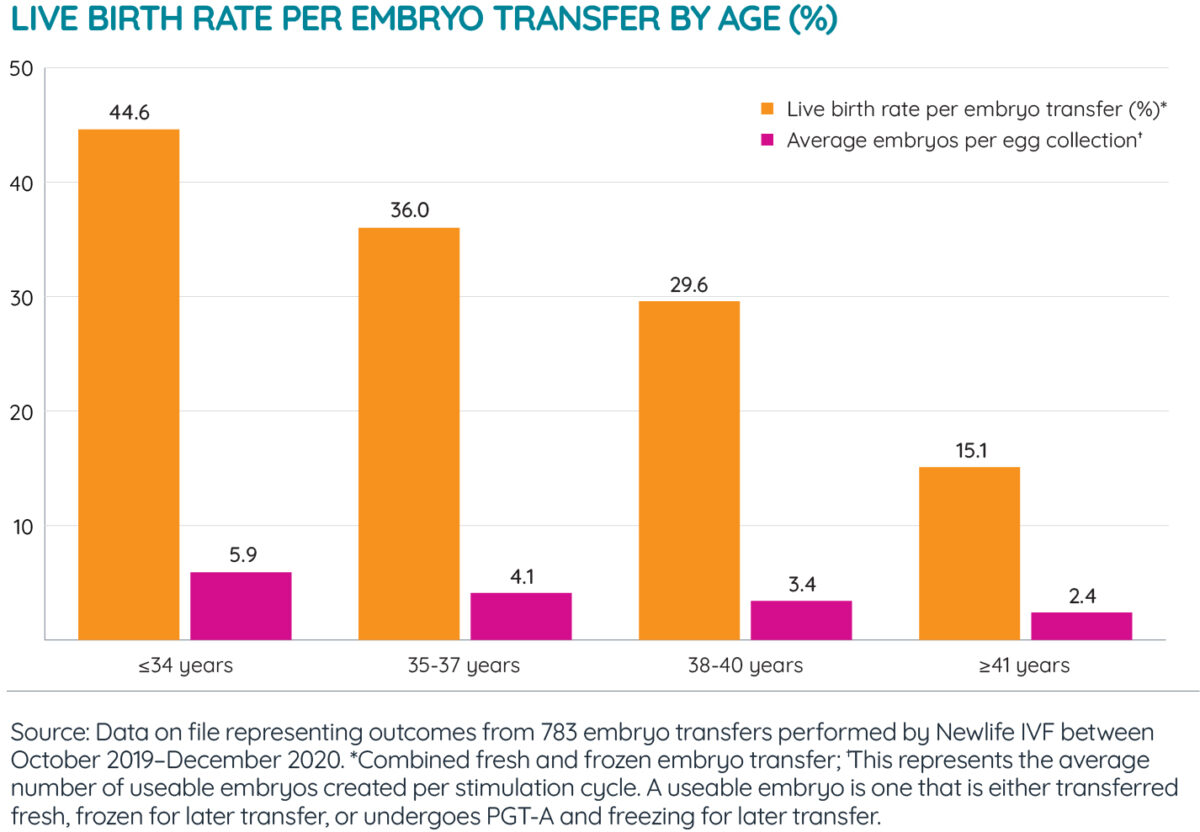
T: (03) 8080 8933 - Success rates
- Fees
Book an appointment
If you’re interested in receiving fertility treatment at Newlife IVF or booking an appointment with one of our fertility specialists
T: (03) 8080 8933 - Resources
Book an appointment
If you’re interested in receiving fertility treatment at Newlife IVF or booking an appointment with one of our fertility specialists
T: (03) 8080 8933 - Blog
Book an appointment
If you’re interested in receiving fertility treatment at Newlife IVF or booking an appointment with one of our fertility specialists
T: (03) 8080 8933 - Locations
Book an appointment
If you’re interested in receiving fertility treatment at Newlife IVF or booking an appointment with one of our fertility specialists
T: (03) 8080 8933 - Contact us